Cancer
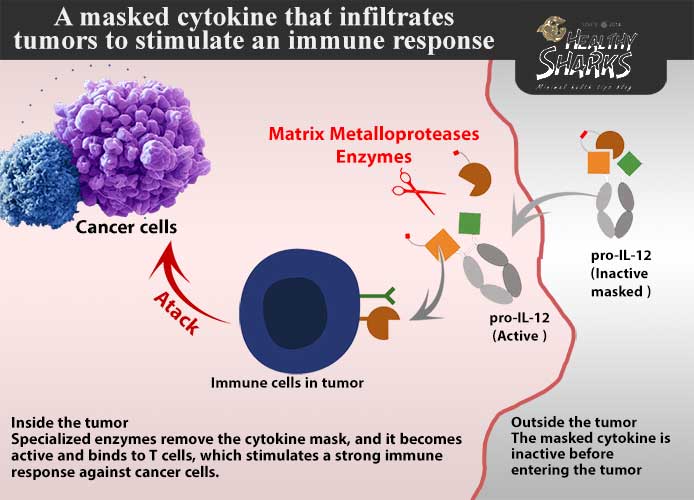
Researchers are developing a modified version of a tumor-infiltrating cytokine to trigger an immune response in specific parts of a patient's body without disrupting the rest of the body.
Despite the tireless efforts made by scientists all over the world to fight cancer, it still claims millions of lives annually, as the number of deaths resulting from infection in 2020 alone reached nearly 10 million cases around the world, and for this reason, scientists are intensifying their efforts to reach More therapeutic strategies that contribute to reducing the incidence of cancer, as well as the search for new treatment methods and techniques.
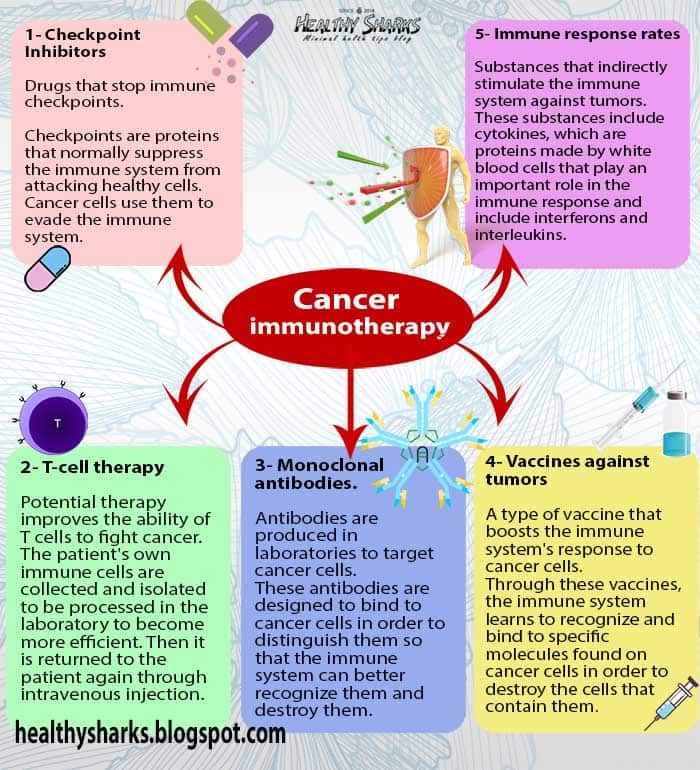
Cancer immunotherapy is one of the promising therapeutic techniques that has made great progress in recent years and is now attracting many research laboratories. The immune system works to protect us from foreign bodies, fight infections and various diseases, and detect and destroy abnormal cells.
Immunotherapy helps the immune system work better against cancer. One type of cancer immunotherapy is "cytokine therapy", which activates the response of immune cells inside tumors, but there are usually unwanted side effects, such as severe toxicity.
In this context, researchers have developed a modified form of cytokines that makes this type of treatment safer, by designing a type of cytokine (IL-12) to target tumors. A powerful addition to our suite of weapons against disease, the same technology may help make other treatments safer.
The research team has been working on this study for nearly six years, according to Benjamin Moon, a researcher at the University of Texas Southwestern Medical Center, and one of the study’s researchers. “Our laboratory is interested in modifying the natural immune molecules in the body to become They are safer and more effective in treating different types of cancer, and one way to do this is to create prodrugs, which are forms of medicine that are activated upon contact with cancer cells.”
Support the immune army
Fighting cancer is part of the normal function of the immune system, for example, tumor-infiltrating lymphocytes or TILs, which are a tool of the immune system, and also a type of white blood cell that migrate from the blood to the tumor and collect around or inside the tumor so that they can kill the cells, However, the cancer cells succeeded in developing defensive methods that enabled them to escape death at the hands of this soldier.
There are several types of cancer immunotherapy, which would help the immune system in its war against the disease. These treatments include different strategies, some of which target the elimination of the defensive methods of cancer cells, and others that aim to enhance and strengthen the immune response and determine its impact to be limited to tumors only.
But immunotherapy can cause side effects when the immune system that's been backed up to fight cancer also works against healthy cells and tissues in the body as well. "The immune cells that can respond and eliminate cancer cells are very much the same as the immune cells in In the blood, where immunotherapies stimulate cells outside the tumor in addition to the cells inside it, non-specific immune stimulation can lead to inflammation and cell death.” For this, researchers focus on several key areas to improve immunotherapy, including how to reduce the side effects of treatment. immune system;
Moon explains: "When you have a cold, most of the symptoms you have, such as a fever, are not from the cold virus, but rather because the immune system is fighting that virus. You can imagine why it would be bad to activate the immune response for the whole body."
Cytokines are proteins made by white blood cells to help the body fight cancer, infection, or other diseases, and they play an important role in the body's immune response.
Mohamed El Gendy Researcher at the Department of Medical Biochemistry and Microbiology at Uppsala University, Sweden says: "Cytokines act as powerful signals that help activate the immune system, but excessive activation causes serious side effects, known as a cytokine storm, and can be fatal, as happened recently with many Covid-19 patients.
Diluted cytokine
Scientists have been able to synthesize these cytokines in the laboratory for use as a treatment for various diseases by helping the immune system kill cancer cells or prevent them from growing. The two main types of cytokines used in cancer treatment are interleukins (ILs) and interferons (INFs).
Mohamed Osama El Orabi, a professor of oncology at Ain Shams University (Egypt), who was not involved in the study says:
"Treatment with interleukins is one of the first therapeutic strategies used in the immunotherapy of tumors - especially kidney tumors and some types of skin cancer - since the 1990s, but the problem that limited the spread of this type was its efficacy and some side effects.
"Cytokines generally stimulate immune cells," Moon says. "Inside tumors, this stimulation activates toxic T cells, which can directly kill cancer cells. Outside the tumor, this stimulation can lead to whole-body inflammation and organ damage.".
Moon and his colleagues wanted to make this type of therapy safer, by developing an interleukin called IL-12. “IL-12 is a powerful cytokine that can completely eliminate tumors in mouse models, although Taking its effective dose is associated with toxic effects, so we wanted to modify the synthesis of IL-12 in a way that would allow us to maintain its effectiveness against tumors, while at the same time reducing the level of toxicity resulting from it.”
The researchers named their improved cytokine pro-IL-12, a cytokine masked that enables it to disguise and infiltrate the tumor to activate antitumor T cells in mice. Once this cytokine enters the tumor, certain tumor-produced enzymes called matrix metalloproteases can remove the mask. Cytokine. Without the mask, the cytokine can stimulate strong immune responses against tumors, as well as slow the growth of various tumors without causing toxic side effects.
Given IL-12's toxicity, the FDA has not authorized its use for cancer treatment, but Moon believes that their study results may represent an important step toward adding cytokines to our anticancer toolkit.
According to the results of the study, the developed cytokine improved the efficacy of therapies targeting tumors in mice, such as treatment with tyrosine kinase inhibitor (TKI) or treatment by inactivating checkpoints, which are promising immunotherapies that are still in their infancy, and the developed cytokine demonstrated similar mechanisms and benefits in tumors. Derived from humans and then transplanted into mice, these findings suggest that pro-IL-12 could have a significant therapeutic effect in cancer patients receiving immunotherapy.
Al-Orabi agrees with that, saying: “This therapeutic strategy may represent a new type of immunotherapy, which may be used alone or in combination with other immunotherapies, but after conducting the necessary clinical trials and approval by the pharmaceutical authorities.”
Obstacles and a long road
Reaching these results was not easy. The researchers encountered many obstacles while designing this new type of prodrug. Moon explained that there was a lot of trial and error until they came up with the perfect design. He also indicated that the secret of their success lay in Finding the right balance between efficacy and toxicity.
It seems that it was worth it. Moon explained that the same technology can be used on other drugs and proteins to make them safer. El Gendy believes that the study offers a promising strategy for developing immunotherapy drugs. He confirms what Moon said, saying: The study provides a versatile strategy that can be used in regimens for other diseases."
The mouse immune system is very different from the human immune system, for example, the balance between neutrophils (neutrophilic granulocytes) and lymphocytes differs greatly between the two types, lymphocytes dominate mouse blood, while neutrophils dominate human blood, according to El Gendy, this is a critical point regarding the results of the Munn study in mice, and adds: “It is expected to see a more pronounced effect of pro-IL-12 use in mice compared to humans, given that pro-IL-12 affects cells lymph".
Moon believes that studies in mice are a starting point for studies in humans, not the end goal, noting that the published data from their study include the use of treated mice provided with human immune cells.
El Gendy also explained that the pro-IL-12 cytokine affects only T cells that are already inside the tumor, but does not cause the migration and infiltration of T cells into the tumor in order to enhance the functioning of the immune system, which raises concerns about the effectiveness of these molecules in clinical studies. “Having a lot of active T cells inside the tumor gives a similar end result,” Moon says in response. “The combination of the pro-IL-12 cytokine we developed with other therapies that stimulate tumor T cell migration but are less effective in activating T cells.” T cells can be particularly effective."
Moon and colleagues are still studying pro-IL-12. "We want to know how the cytokine we've developed works, what cells it affects, and what we can do more to improve its effect," Moon says. These questions can help us identify patients For whom this type of therapy is better suited, and may help design better prodrugs for the future, we are working to develop some other cytokines that may have medical applications if we can control their toxicity as well.”
“El Gendy” stressed the need to conduct studies that determine the best dose of the drug, and determine the maximum permissible dose, before moving to the clinical trial stage, which Moon agreed with, saying: “This type of studies must be conducted at some point, given the fact that We are still in the early stages of the design and mechanistic studies, so it may be a bit premature, at the moment, we only tested the cytokine on mice, and it may undergo further changes to its design.”
El Gendy also emphasized that the strategy used in the current study provides insight into multiple uses for better drug development, and explained that reaching a balanced immune response may help treat critical cases of COVID-19 as well, by avoiding the cytokine storm.
















0 comments:
Post a Comment